DISCOVER
Discover the latest news, articles, and publications featuring Butter BV and key developments in everyday infections. Here you’ll find updates on research, innovations, and progress in improving treatment access, diagnostics, and care pathways.

New Evidence on Hydrogen Peroxide Cream for Impetigo (TIARA Trial)
A large clinical study from New Zealand—the TIARA trial—has provided new insights into the use of hydrogen peroxide (H₂O₂) cream for treating non-severe impetigo in children. The trial compared H₂O₂ cream with the commonly used topical antibiotic fusidic acid.
While H₂O₂ was slightly less effective overall, the difference was small, and for children with localized impetigo, the treatment performed similarly to the antibiotic. The study also confirmed that H₂O₂ is safe, with only one mild skin reaction reported and no systemic side effects.
Importantly, the researchers highlight that using antiseptics like H₂O₂ may help reduce antibiotic use and slow the development of antimicrobial resistance, which is increasingly important in the management of common skin infections.
These findings support the role of hydrogen peroxide cream as a reasonable, accessible option for non-severe, localized impetigo—particularly in settings aiming to limit unnecessary antibiotic exposure.
*Topical hydrogen peroxide versus fusidic acid for non-severe impetigo in Auckland, Aotearoa New Zealand (the TIARA trial): a single-blind, randomised controlled trial. Primhak et al. The Lancet Primary Care, Volume 1, Issue 5, 100054
New Study Shows Rapid Rise in Scabies and Growing Pressure on Primary Care
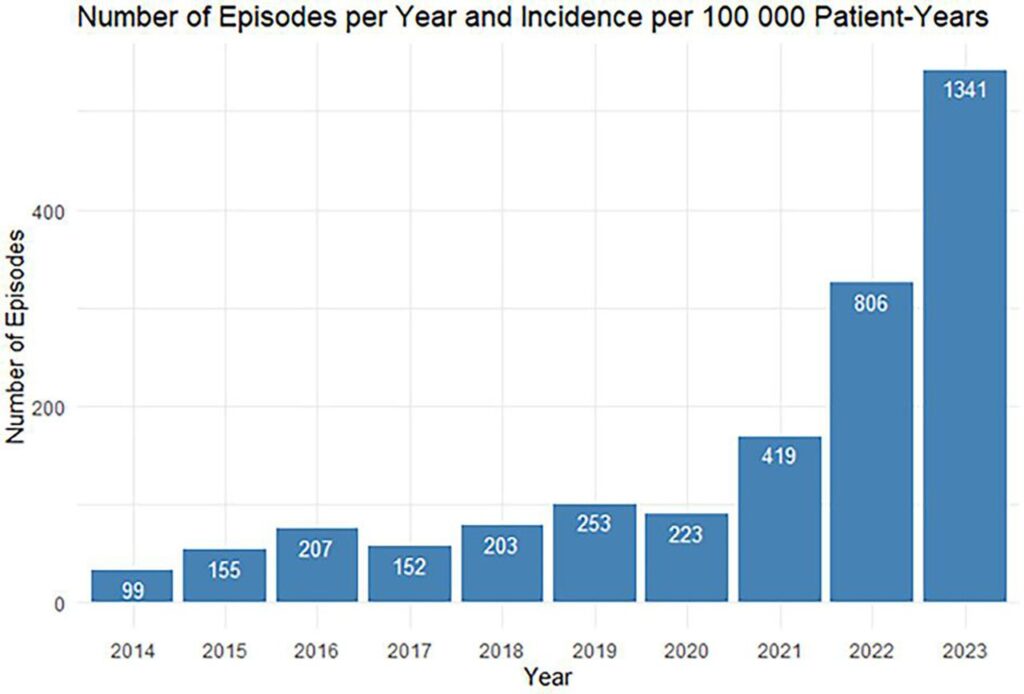
A new Dutch study published in BJGP Open reveals a sharp rise in scabies cases over the past decade, placing increasing pressure on general practitioners. Using data from nearly 40,000 patients, researchers found that scabies-related episodes increased more than 13-fold between 2014 and 2023—from 99 to 1341 episodes per 100,000 patient-years.
The number of GP encounters for scabies rose in parallel, with young adults (17–25 years) showing the largest increase. Doctors are diagnosing scabies faster than before, but the overall workload has grown substantially, with more consultations, prescriptions, and referrals needed to manage cases.
The study concludes that the rising incidence represents a significant and urgent public health challenge. Improved diagnostics, better preventive measures, and more coordinated public health action are needed to limit transmission and reduce the strain on healthcare services.
For Butter BV, these findings underscore the importance of developing simple, accessible tools and innovative approaches to reduce the burden of everyday infections—including scabies—on patients, clinicians, and society.
*Rising scabies incidence and the growing burden on GPs: a retrospective longitudinal study. van der Boor et al. BJGP Open 2 December 2025; BJGPO.2025.0037

Rising Fusidic Acid Resistance in Common Skin Infections
Recent reports from the Dutch National Institute for Public Health and the Environment show an increase in cases of Staphylococcus aureus that are resistant to fusidic acid—a topical antibiotic commonly used to treat impetigo and other skin infections in primary care. Surveillance data indicate that both fusidic-acid-resistant S. aureus and fusidic-acid-resistant MRSA are being found more frequently in wound and skin cultures, with especially notable increases reported among children in recent years.
Because fusidic acid may be less effective when resistance is present, doctors are advised to be alert for treatment failure and consider further testing. This trend highlights the broader challenge of antibiotic resistance in everyday infections, and the need for alternative strategies, better diagnostics, and evidence-based treatment options. For Butter BV, developments like this underscore the importance of advancing practical, accessible solutions that can help reduce unnecessary antibiotic use and improve infection care pathways.
www.nhg.org/actueel/toename-van-fusidinezuurresistente-s-aureus/

Study Shows Limited Accuracy of Dipstick Tests for UTIs in Pregnancy
A new Dutch study published in Antibiotics examined how well urine dipstick tests work for diagnosing urinary tract infections (UTIs) in pregnant women. Although dipsticks are widely used because they are quick and simple, the study found that in real-world practice, their accuracy is much lower than previously reported.
Out of 718 urine samples, only 6.8% actually showed a confirmed infection on culture, even though many dipstick results were positive. The commonly used markers—leukocyte esterase and nitrite—missed some infections but also produced many false positives, leading to unnecessary antibiotic treatment. Notably, among pregnant women given nitrofurantoin for a suspected UTI, only 16.8% had a positive culture confirming the diagnosis.
The authors conclude that dipsticks alone are not reliable for diagnosing UTIs in pregnancy and can contribute to overtreatment, exposing women and babies to antibiotics they may not need.
For Butter BV, these findings highlight the importance of better diagnostic tools, smarter care pathways, and reducing unnecessary antibiotic use—key steps in improving the management of everyday infections.
Diagnostic Accuracy of Urine Dipsticks for Urinary Tract Infection Diagnosis during Pregnancy: A Retrospective
Cohort Study. Werter et al. Antibiotics 2024, 13, 567
